Fixed prostheses on natural teeth are now a common rehabilitation treatment capable of restoring lost dental structure, tooth shape, function and aesthetics. (1) Although the gold standard is still represented by metal-ceramic restorations, all-ceramic solutions are gaining popularity, thanks to their better aesthetic properties, biocompatibility and mechanical characteristics. (2)
Many types of preparation have been proposed in fixed prosthetics, both in clinical practice and in the literature.
In general, the preparation types can be classified as horizontal or vertical. (3)
Despite all the types of preparation available, horizontal ones are often preferred by clinicians for very practical reasons. In fact, horizontal preparations are more visible on the prepared tooth, in the impression and on the plaster model and ensure that the margins of the temporary and final prosthesis are clearer and more precise. (1)
Vertical preparations, on the other hand, offer worse marginal adaptation and the presence of prosthetic over-contours. (4)
However, vertical preparations lead to smaller gaps between the abutment and the restoration, while inflammation in the gingival sulcus area may be reduced. (5)
Horizontal prosthetic preparations
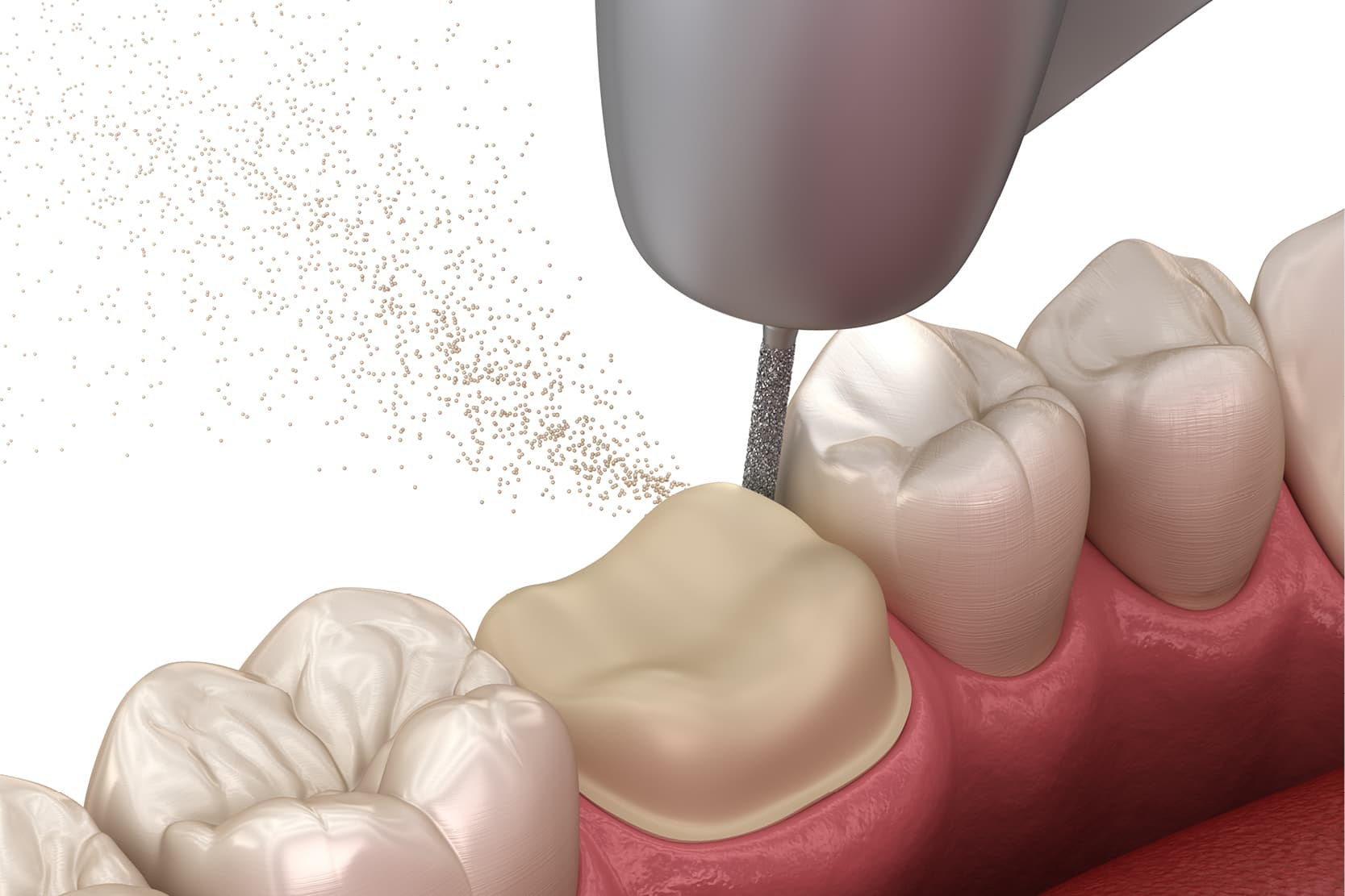
Horizontal prosthetic preparations are characterised by the presence of a clear, defined and legible line of the preparation finish. There are many possible designs in this context, each with specific characteristics, suitable for specific materials and obtainable with the use of specific diamond cutters. The most common horizontal preparation designs are chamfer and shoulder.
The horizontal preparation by definition is represented by the shoulder preparation, which can be at 90° (angle between the vertical axis and the horizontal component of the preparation) as well as at 50°, or with different angles between the two components, the axial and the “horizontal”.
Chamfer: features and advantages
The chamfer is instead characterised by a curved finishing line, without any sharp corners. This “soft” line improves stress distribution and is ideal for both metal-ceramic and all-ceramic crowns. (6) Chamfer preparation lines are also well suited for digital workflows since any sharp corners represent a possible source of distortions and inaccuracies both in the scanning phase and in the CAM production phase. (7)
In general, horizontal preparations (shoulder and chamfer) allow the dental technician to precisely locate the finishing margin and can therefore easily “read” the preparation and position the prosthetic margin with maximum precision.
Furthermore, the horizontal preparation offers more prosthetic space at the margin level, thus allowing for the necessary thickness for both the metal structure and the ceramic layer.
Vertical prosthetic preparations
Vertical dental preparations represent an evolution in prosthetic rehabilitation. Unlike horizontal preparations, which provide well-defined margins (chamfer or shoulder), the vertical preparation eliminates the finished margin, allowing greater freedom in the management of soft tissues and in the position of the prosthetic margin (8).
Having a preparation area instead of a clear margin essentially allows the latter to be moved more or less apically, provided that its biological width is respected. This feature is particularly useful when the clinical crown does not match the anatomical crown or when it is desirable to change the shape and volume of the prosthetic emergence profile.
The preservation of healthy dental tissue is one of the main advantages of this technique. The lack of a horizontal margin reduces the amount of dentin removed, decreasing the risk of pulp complications (3). Furthermore, the possibility of shaping the emergence profile through customised temporaries allows for a better aesthetic and functional integration with the periodontal tissues, promoting the stability of the gingival margin (9). The subgingival prosthetic margin can be positioned in a biologically compatible manner, adapting to the new tissue architecture.
Limitations and clinical difficulties of vertical dental preparations
However, there are some disadvantages. The technique is highly sensitive and requires considerable clinical experience. Control of the subgingival finish line can be complex and depends on extremely precise impressions obtained with double-cord gingival retraction techniques (3). Furthermore, communication between the clinician and the dental technician must be optimal to ensure a functional and predictable result.
However, not having a preparation thickness at the margin level also leads to another significant issue: however much the thickness of the restoration can be reduced, by definition there will always be a point where we will have a prosthetic over-contour.
Vertical dental preparation therefore offers important benefits in terms of tissue conservation and aesthetics, but requires operational precision and advanced skills.
In conclusion, it is clear that no type of preparation is superior to another. For each clinical scenario and based on the material to be used, the dentist will be able to explore different types of preparation guided by predominantly clinical and rehabilitative considerations.
- Bonfanti#LioxSpecialChar8208#Gris, M., Pradies, G., Moron#LioxSpecialChar8208#Conejo, B., Gil, A., & Martinez#LioxSpecialChar8208#Rus, F. (2025). Vertical Versus Horizontal Finishing Lines for Dental Preparations: A Systematic Review With Meta#LioxSpecialChar8208#Analysis. Journal of Esthetic and Restorative Dentistry, 37(3), 707-726.
- Sirous, S., Navadeh, A., Ebrahimgol, S., & Atri, F. (2022). Effect of preparation design on marginal adaptation and fracture strength of ceramic occlusal veneers: A systematic review. Clinical and Experimental Dental Research, 8(6), 1391-1403.
- Agustín-Panadero, R., Serra-Pastor, B., Fons-Font, A., & Solá-Ruíz, M. F. (2018). Prospective clinical study of zirconia full-coverage restorations on teeth prepared with biologically oriented preparation technique on gingival health: results after two-year follow-up. Operative Dentistry, 43(5), 482-487.
- Scutellà, F., Weinstein, T., Zucchelli, G., Testori, T., & Fabbro, M. D. (2017). A Retrospective Periodontal Assessment of 137 Teeth After Featheredge Preparation and Gingittage. International Journal of Periodontics & Restorative Dentistry, 37(6).
- Comlekoglu, M., Dundar, M., Özcan, M., Gungor, M., Gokce, B., & Artunc, C. (2009). Influence of cervical finish line type on the marginal adaptation of zirconia ceramic crowns. Operative dentistry, 34(5), 586-592.
- Shillingburg Jr, H. T., Sather, D. A., Wilson Jr, E. L., Cain, J. R., Mitchell, D. L., & Blanco, L. J. (2012). Fundamentals of fixed prosthodontics. 4th. Chichago, IL, USA: Quintessence.
- Bindl, A., & Mörmann, W. H. (2005). Marginal and internal fit of all#LioxSpecialChar8208#ceramic CAD/CAM crown#LioxSpecialChar8208#copings on chamfer preparations. Journal of oral rehabilitation, 32(6), 441-447.
- Loi, I., & Di Felice, A. (2013). Biologically oriented preparation technique (BOPT): A new approach for prosthetic restoration of periodontically healthy teeth. European Journal of Esthetic Dentistry, 8(1), 10–23.
- Zarone, F., Sorrentino, R., Traini, T., Di Mauro, M. I., & Ferrari, M. (2019). Prosthetic treatment strategies with the biologically oriented preparation technique. International Journal of Esthetic Dentistry, 14(1), 16–33
Would you like more information about Zhermack Dental products and solutions?
Contact us




 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


