In the past few years, additive manufacturing technologies, commonly known as 3D printing – also rapid prototyping, layered manufacturing, eManufacturing or free form manufacturing – have been increasingly applied in dentistry, profoundly transforming clinical and, in particular, laboratory practice.
The possibility of producing customised devices, sometimes at low cost, with high accuracy, quickly and in any required shape, has opened up new prospects in the various dental sectors (1).
However, to be able to apply these technologies properly, it is necessary to understand their technical differences, potential applications and limitations.
Types of 3D printing technologies
The International Organization for Standardization has classified the different additive technologies into 7 categories (2):
- Vat polymerisation
- Material extrusion technology
- Material jetting technology
- Binder jetting technology
- Powder-bed fusion
- Sheet lamination
- Direct energy deposition
The technologies above can also be classified on the basis of the physical state in which the material they use is printed, which can be in the form of a liquid, filamentous/paste, powder or solid laminated sheets. (3)
Vat polymerisation: the most precise 3D printing techniques
Vat polymerisation techniques can themselves be divided into (1,4):
- Stereolithography (SLA)
- Direct Light Processing (DLP)
- Liquid Crystal Display (LCD)
- Continuous Liquid Interface Production (CLIP)
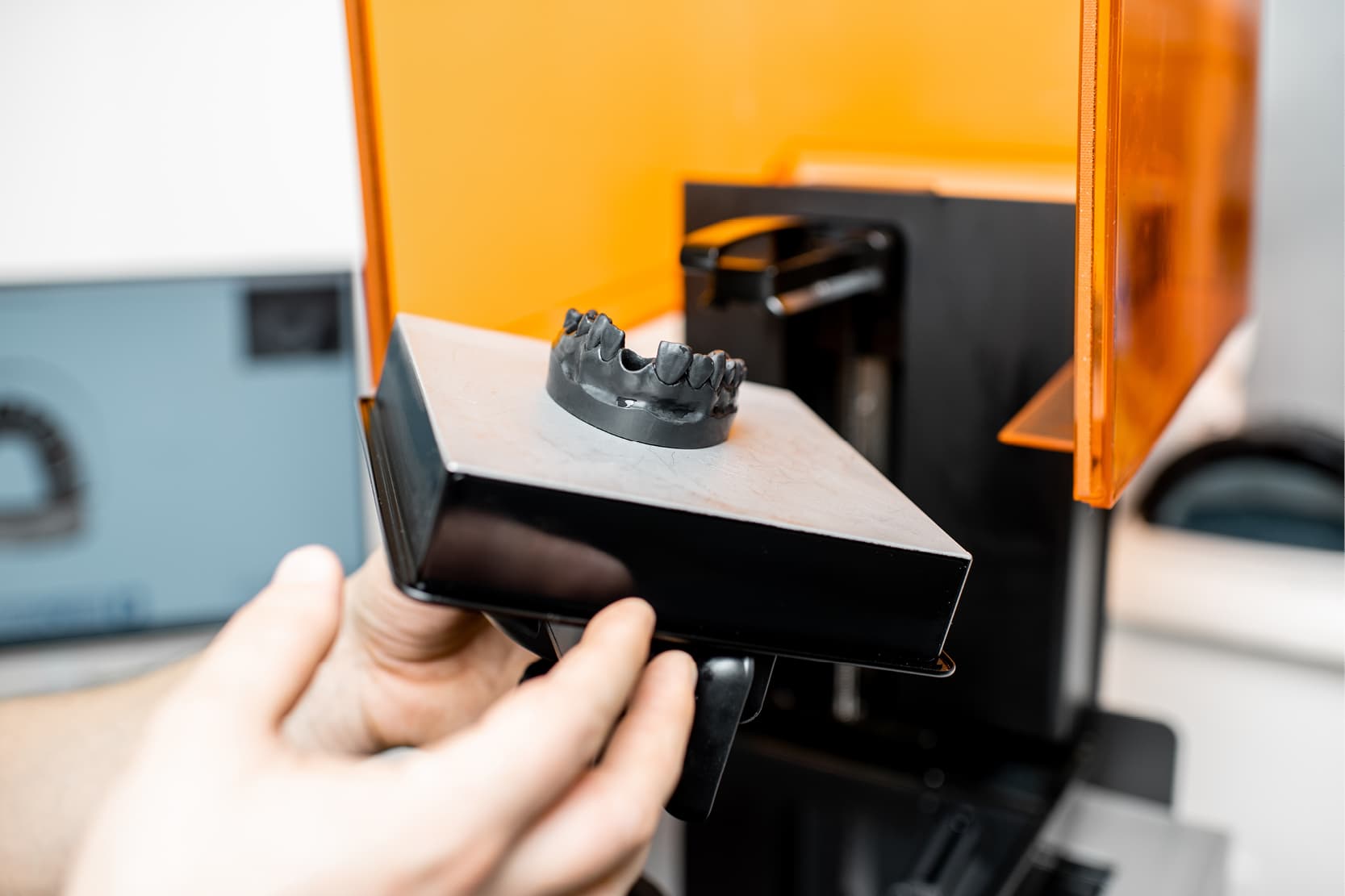
Stereolithography (SLA) involves the photopolymerisation of liquid resins using a beam of UV light. Photopolymer resins contain a photo-initiator which, when activated by UV light, releases a catalyst capable of starting the polymerisation reaction.
In practice, the photo-initiator splits into multiple particles that react with the monomers (and/or oligomers), binding them together to form polymers (4). This technology offers high resolution and detail, making it particularly suitable for dental models, surgical guides and temporary restorations (5,6).
A similar option, DLP, uses a different light source (usually a projector) to cure entire layers of resin in a single exposure, further reducing print times. This technology uses special micromirrors which direct the reflection of the polymerising light in order to generate the shape of the layer determined in advance by the slicing software (7,8).
On the other hand, LCD uses a screen containing pixels which can be opened or closed depending on the shape of the section to be printed (9). In CLIP, UV light passes through a transparent window beneath which a thin layer of oxygen-rich resin forms that does not polymerise, called the “dead zone”. Above this, the oxygen-free resin begins to polymerise following the pattern of the projected 2D cross-sections (1). These techniques can be used to produce models, templates for guided surgery and even bases for total removable prostheses (7,10,11).
Additive manufacturing technologies: FDM and SLS/SLM laser systems
In the case of Fused deposition modeling (FDM), this is one of the most accessible technologies, thanks to the low cost of printers and materials (12). With this technique, a thermoplastic filament is melted and deposited layer by layer until the object is formed. Although it has a lower dimensional accuracy than SLA or DLP, FDM can be useful in producing diagnostic models or for preliminary testing (12).
More advanced technologies such as selective laser sintering (SLS) and selective laser melting (SLM) use a high-power laser to sinter or melt powders, usually of metallic materials (13,14).
In the dental field, SLM is mainly used for the production of chromium-cobalt frameworks for fixed prostheses on teeth and implants or for implant components (13,14). These systems enable the production of complex, highly resistant shapes with geometries as precise as milled parts (15). However, they require specific design skills and the component produced needs to undergo a final heat treatment to reduce the residual stresses generated by the high temperature gradients reached (16).
Clinical applications of 3D printing in dentistry
Nowadays, there are many clinical applications of 3D printing, with their number steadily growing. In prosthetics, the ability to produce customised crowns, bridges and customised implant structures has reduced processing times and increased accuracy in terms of marginal fit (17).
In orthodontics, 3D printing provides the basis for producing models for clear aligners and auxiliary devices. In oral surgery, surgical guides improve the predictability of implant interventions, while printed anatomical models support planning (18).
However, integrating 3D printing into dental practice also brings some challenges. It is essential for professionals to acquire advanced digital skills, not only in the use of printers but also in CAD workflows and slicing software.
Furthermore, it is necessary to consider the initial financial investment, the costs of materials and the management of post-curing processes, which are fundamental to finalising the workflow. Finally, particular attention should be paid to the medical regulatory framework: 3D printed devices must comply with the European MDR regulations and, where applicable, be accompanied by a CE mark (1).
In conclusion, 3D printing has become one of the key technologies in the evolution of digital dentistry, paving the way for an increasingly personalised, efficient and precise clinical practice which, however, must always be accompanied by suitable training for all dental staff.
References:
1. Alammar A, Kois JC, Revilla-León M, Att W. Additive Manufacturing Technologies: Current Status and Future Perspectives. J Prosthodont. 2022 Mar;31(S1):4–12.
2. ISO/ASTM 52900:2015, Additive manufacturing — General principles — Terminology.
3. Kruth JP, Leu MC, Nakagawa T. Progress in Additive Manufacturing and Rapid Prototyping. CIRP Annals. 1998 Jan 1;47(2):525–40.
4. Revilla-León M, Özcan M. Additive Manufacturing Technologies Used for Processing Polymers: Current Status and Potential Application in Prosthetic Dentistry. J Prosthodont. 2019 Feb;28(2):146–58.
5. Alharbi N, Osman RB, Wismeijer D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int J Prosthodont. 2016 Oct;29(5):503–10.
6. D’haese J, Van De Velde T, Elaut L, De Bruyn H. A Prospective Study on the Accuracy of Mucosally Supported Stereolithographic Surgical Guides in Fully Edentulous Maxillae: Mucosally Supported Stereolithographic Surgical Guides. Clin Implant Dent Rel Res. 2012 Apr;14(2):293–303.
7. Yoon HI, Hwang HJ, Ohkubo C, Han JS, Park EJ. Evaluation of the trueness and tissue surface adaptation of CAD-CAM mandibular denture bases manufactured using digital light processing. J Prosthet Dent. 2018 Dec;120(6):919–26.
8. Reich S, Berndt S, Kühne C, Herstell H. Accuracy of 3D-Printed Occlusal Devices of Different Volumes Using a Digital Light Processing Printer. Appl Science. 2022 Jan;12(3):1576.
9. Tseng CW, Lin WS, Sahrir CD, Lin WC. The impact of base design and restoration type on the resin consumption, trueness, and dimensional stability of dental casts additively manufactured from liquid crystal display 3D printers. J Prosthodont. n/a(n/a).
10. Kalberer N, Mehl A, Schimmel M, Müller F, Srinivasan M. CAD-CAM milled versus rapidly prototyped (3D-printed) complete dentures: An in vitro evaluation of trueness. J Prosthet Dent. 2019 Apr;121(4):637–43.
11. Grande F, Pavone L, Molinelli F, Mussano F, Srinivasan M, Catapano S. CAD-CAM complete digital dentures: An improved clinical and laboratory workflow. J Prosthet Dent. 2024 Dec 28;S0022-3913(24)00821-7.
12. Moby V, Dupagne L, Fouquet V, Attal JP, François P, Dursun E. Mechanical Properties of Fused Deposition Modeling of Polyetheretherketone (PEEK) and Interest for Dental Restorations: A Systematic Review. Materials (Basel). 2022 Sep 30;15(19):6801.
13. Li J, Chen C, Liao J, Liu L, Ye X, Lin S, et al. Bond strengths of porcelain to cobalt-chromium alloys made by casting, milling, and selective laser melting. J Prosthet Dent. 2017 Jul;118(1):69–75.
14. Revilla-León M, Ceballos L, Martínez-Klemm I, Özcan M. Discrepancy of complete-arch titanium frameworks manufactured using selective laser melting and electron beam melting additive manufacturing technologies. J Prosthet Dent. 2018 Dec 1;120(6):942–7.
15. Revilla-León M, Ceballos L, Özcan M. Implant Prosthodontic Discrepancy of Complete-Arch Co-Cr Implant Frameworks Manufactured Through Selective Laser Melting Additive Manufacturing Technology Using a Coordinate Measuring Machine. Int J Oral Maxillofac Implants. 2019;34(3):698–707.
16. Korkmaz ME, Gupta MK, Waqar S, Kuntoğlu M, Krolczyk GM, Maruda RW, et al. A short review on thermal treatments of Titanium & Nickel based alloys processed by selective laser melting. Journal of Materials Research and Technology. 2022 Jan 1;16:1090–101.
17. Revilla-León M, Sánchez-Rubio JL, Pérez-López J, Rubenstein J, Özcan M. Discrepancy at the implant abutment-prosthesis interface of complete-arch cobalt-chromium implant frameworks fabricated by additive and subtractive technologies before and after ceramic veneering. J Prosthet Dent. 2021 May;125(5):795–803.
18. D’haese R, Vrombaut T, Hommez G, De Bruyn H, Vandeweghe S. Accuracy of Guided Implant Surgery Using an Intraoral Scanner and Desktop 3D-Printed Tooth-Supported Guides. Int J Oral Maxillofac Implants. 2022 May;37(3):479–84.
Would you like more information about Zhermack Dental products and solutions?
Contact us



 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


