Artificial Intelligence (AI) is “a computerised process that aims to reproduce human or animal intelligence and that is applied in a vast range of fields (for example, automatic learning, natural language processing and robotics)” [1].
It is already applied in a vast spectrum of disciplines, not only within the field of medicine, but also in mathematics, finance, engineering and business [2].
However, the purpose and mode of application of artificial intelligence are always the same: the imitation of the human decision-making process by establishing correlations and principles as a result of a logical use and mathematical analysis of the source data.
Human decisions should thus theoretically be facilitated and more accurate, since all the aspects, the pros and cons relating to a given issue or illness, are taken into account by the machine that, after sifting through all the data available, processes the best solution [3,4].
Personalised and preventive “precision medicine”
In the field of medicine, artificial intelligence could therefore lead to a better understanding of illness in the various populations of the world and different individuals through the computerised analysis and extrapolation of a vast range of data.
This would make it possible to achieve “precision medicine”, i.e. personalised medicine based on preventive and therapeutic interventions not on a large scale but targeted to specific individuals.
It is a form of medicine that takes into account individual differences in genetics, lifestyle, diet and family history, thus making it possible to identify the therapies best suited to the individual clinical case [5].
(h2) Predictive dentistry and diagnostic imaging: the role of AI
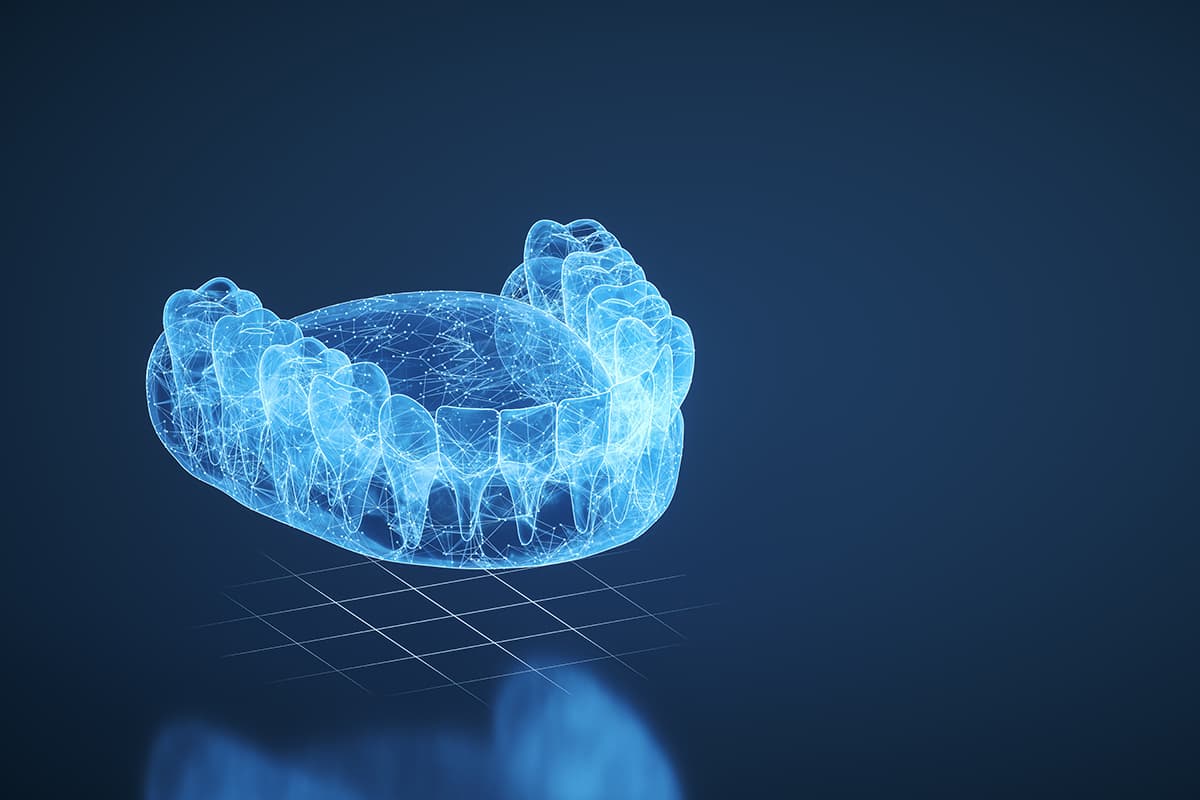
In the field of dentistry, by exploiting the basic principles of deep learning, artificial intelligence is starting to make its way into activities and programmes regarding predictive dentistry and diagnosticimaging [6].
In orthodontics, certain programmes already allow the automatic detection of cephalometric landmarks on latero-lateral teleradiography of radiographic changes resulting from non-extractive orthodontic treatments and growth and development forecasts [7,8].
AI in radiographic analysis
In conservative dentistry, artificial intelligence mechanisms are applied primarily in the analysis of endoral X-rays for diagnosing interproximal and enamel caries and to understand the actual extent of dentin involvement [9]. Greyscale analysis for the different pixels in X-rays is in fact used to discriminate the presence or absence of caries and their size.
Following the same principle, analysing endoral X-rays allows some AI systems to detect endodontic disease and read the anatomy of the root canals, giving an idea of the difficulty of possible root canal therapy [10].
Again in relation to radiographic analysis, in periodontics and implantology artificial intelligence proves useful for understanding the types of bone defect present and for assessing the risk of developing periodontal/peri-implant disease, following, for example, the observation of the disappearance of the lamina dura [11,12].
Furthermore, deep learning in this field can also allow the recognition of the type of implant present in the bone, in the case of a patient who has an implant the type of which is not known [13].
AI in prosthetic and maxillofacial settings
In the prosthetic field, occlusal analysis and parafunctional sign recognition are currently still in the experimental phase, although the preliminary studies are encouraging [14].
In maxillofacial surgery, on the other hand, artificial intelligence is useful for planning cases of orthognathic and oncological surgery [15]. Further applications make it possible to assess the extent of maxillary osteonecrosis using CBCT [16].
The diagnosis of temporomandibular problems of anatomical origin and squamous cell carcinoma of the buccal mucosae could also benefit from the application of deep learning algorithms [17,18].
Prospects and limits of AI in dentistry
The above-mentioned uses are just the start of the possible application of artificial intelligence in dentistry. However, although in certain respects these algorithms are accurate and precise, they also have some limits.
For example, the indication by artificial intelligence systems of the hard and soft tissue landmarks in the menton and pogonion areas on cephalometric X-rays is often inaccurate, because the position and tilt of the chin are difficult to predict based on a profile X-ray or picture [14].
Furthermore, the steps regarding the reconstruction of the CBCT image, the segmentation process and surgical planning are still delicate steps in whichdeep learning algorithms can make errors, the consequences of which can be serious [15].
It is also necessary to understand the mechanism by which the algorithms work[3,4] and, given the complexity of this new technology and the intrinsic critical issues regarding its use in medical field, it cannot be ruled out that new professional medical roles will emerge in the future [19].
The use of AI in dentistry will undoubtedly have a significant impact, which must, however, be evaluated depending on the branch and the clinical and extra-clinical application of the software in this field.
References
[1] Ramesh AN, Kambhampati C, Monson JRT, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl 2004;86:334–8. https://doi.org/10.1308/147870804290.
[2] Borana J. Applications of Artificial Intelligence & Associated Technologies, 2016.
[3] Mohammad-Rahimi H, Rokhshad R, Bencharit S, Krois J, Schwendicke F. Deep learning: A primer for dentists and dental researchers. J Dent 2023;130:104430. https://doi.org/10.1016/j.jdent.2023.104430.
[4] Ducret M, Mörch C-M, Karteva T, Fisher J, Schwendicke F. Artificial intelligence for sustainable oral healthcare. J Dent 2022;127:104344. https://doi.org/10.1016/j.jdent.2022.104344.
[5] König IR, Fuchs O, Hansen G, von Mutius E, Kopp MV. What is precision medicine? Eur Respir J 2017;50:1700391. https://doi.org/10.1183/13993003.00391-2017.
[6] Schwendicke F, Krois J. Data Dentistry: How Data Are Changing Clinical Care and Research. J Dent Res 2022;101:21–9. https://doi.org/10.1177/00220345211020265.
[7] Park JH, Kim Y-J, Kim J, Kim J, Kim I-H, Kim N, et al. Use of artificial intelligence to predict outcomes of nonextraction treatment of Class II malocclusions. Seminars in Orthodontics 2021;27:87–95. https://doi.org/10.1053/j.sodo.2021.05.005.
[8] Mohammad-Rahimi H, Nadimi M, Rohban MH, Shamsoddin E, Lee VY, Motamedian SR. Machine learning and orthodontics, current trends and the future opportunities: A scoping review. American Journal of Orthodontics and Dentofacial Orthopedics 2021;160:170-192.e4. https://doi.org/10.1016/j.ajodo.2021.02.013.
[9] Mohammad-Rahimi H, Motamedian SR, Rohban MH, Krois J, Uribe SE, Mahmoudinia E, et al. Deep learning for caries detection: A systematic review. Journal of Dentistry 2022;122:104115. https://doi.org/10.1016/j.jdent.2022.104115.
[10] Sadr S, Mohammad-Rahimi H, Motamedian SR, Zahedrozegar S, Motie P, Vinayahalingam S, et al. Deep Learning for Detection of Periapical Radiolucent Lesions: A Systematic Review and Meta-analysis of Diagnostic Test Accuracy. Journal of Endodontics 2023;49:248-261.e3. https://doi.org/10.1016/j.joen.2022.12.007.
[11] Revilla-León M, Gómez-Polo M, Barmak AB, Inam W, Kan JYK, Kois JC, et al. Artificial intelligence models for diagnosing gingivitis and periodontal disease: A systematic review. The Journal of Prosthetic Dentistry 2022. https://doi.org/10.1016/j.prosdent.2022.01.026.
[12] Mohammad-Rahimi H, Motamedian SR, Pirayesh Z, Haiat A, Zahedrozegar S, Mahmoudinia E, et al. Deep learning in periodontology and oral implantology: A scoping review. Journal of Periodontal Research 2022;57:942–51. https://doi.org/10.1111/jre.13037.
[13] Revilla-León M, Gómez-Polo M, Vyas S, Barmak BA, Galluci GO, Att W, et al. Artificial intelligence applications in implant dentistry: A systematic review. J Prosthet Dent 2023;129:293–300. https://doi.org/10.1016/j.prosdent.2021.05.008.
[14] Farook TH, Rashid F, Ahmed S, Dudley J. Clinical machine learning in parafunctional and altered functional occlusion: A systematic review. J Prosthet Dent 2023:S0022-3913(23)00051-3. https://doi.org/10.1016/j.prosdent.2023.01.013.
[15] Minnema J, Ernst A, van Eijnatten M, Pauwels R, Forouzanfar T, Batenburg KJ, et al. A review on the application of deep learning for CT reconstruction, bone segmentation and surgical planning in oral and maxillofacial surgery. Dentomaxillofacial Radiology 2022;51. https://doi.org/10.1259/dmfr.20210437.
[16] Wongratwanich P, Shimabukuro K, Konishi M, Nagasaki T, Ohtsuka M, Suei Y, et al. Do various imaging modalities provide potential early detection and diagnosis of medication-related osteonecrosis of the jaw? A review. Dentomaxillofacial Radiology 2021;50. https://doi.org/10.1259/dmfr.20200417.
[17] Jha N, Lee K, Kim Y-J. Diagnosis of temporomandibular disorders using artificial intelligence technologies: A systematic review and meta-analysis. PLOS ONE 2022;17:e0272715. https://doi.org/10.1371/journal.pone.0272715.
[18] Alabi RO, Youssef O, Pirinen M, Elmusrati M, Mäkitie AA, Leivo I, et al. Machine learning in oral squamous cell carcinoma: Current status, clinical concerns and prospects for future—A systematic review. Artificial Intelligence in Medicine 2021;115:102060. https://doi.org/10.1016/j.artmed.2021.102060.
[19] Cussat-Blanc S, Castets-Renard C, Monsarrat P. Doctors in Medical Data Sciences: A New Curriculum. International Journal of Environmental Research and Public Health 2023;20:675. https://doi.org/10.3390/ijerph20010675.
Do you want more information on Zhermack Dental products and solutions?
Contact us



 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


