Enamel-dentin adhesion has been a true revolution in dentistry, a paradigm shift that effectively transformed an entire approach. Thanks to the constant improvement of techniques and materials and the discovery of more effective protocols, in just a few years we have moved from “retentive” dentistry to adhesive dentistry.
Dentistry is gradually becoming less and less invasive thanks to this sudden change in perspective. In fact, although a restoration once stayed in place because it was supported by mechanical retention and/or a certain degree of undercut, which had to be achieved by sacrificing part of the tooth structure, it is now possible to count on a new ally: enamel-dentin adhesion.
Among the fundamental aspects of adhesive dentistry is adhesion to enamel and dentin, which poses profoundly different challenges due to the microstructural and compositional differences of these two substrates.
Structure and composition of enamel and dentin
Enamel is the most mineralised tissue in the human body, composed of approximately 96% minerals (hydroxyapatite), 1% organic material and 3% water (1). It is highly crystalline and has a prismatic structure.
Dentin, on the other hand, is a hydrated tissue, rich in collagen, composed of approximately 70% minerals, 20% organic material (type I collagen) and 10% water (2). The dentin is criss-crossed by dentinal tubules whose density and diameter progressively increase as they approach the pulp chamber.
Mechanisms of adhesion to enamel
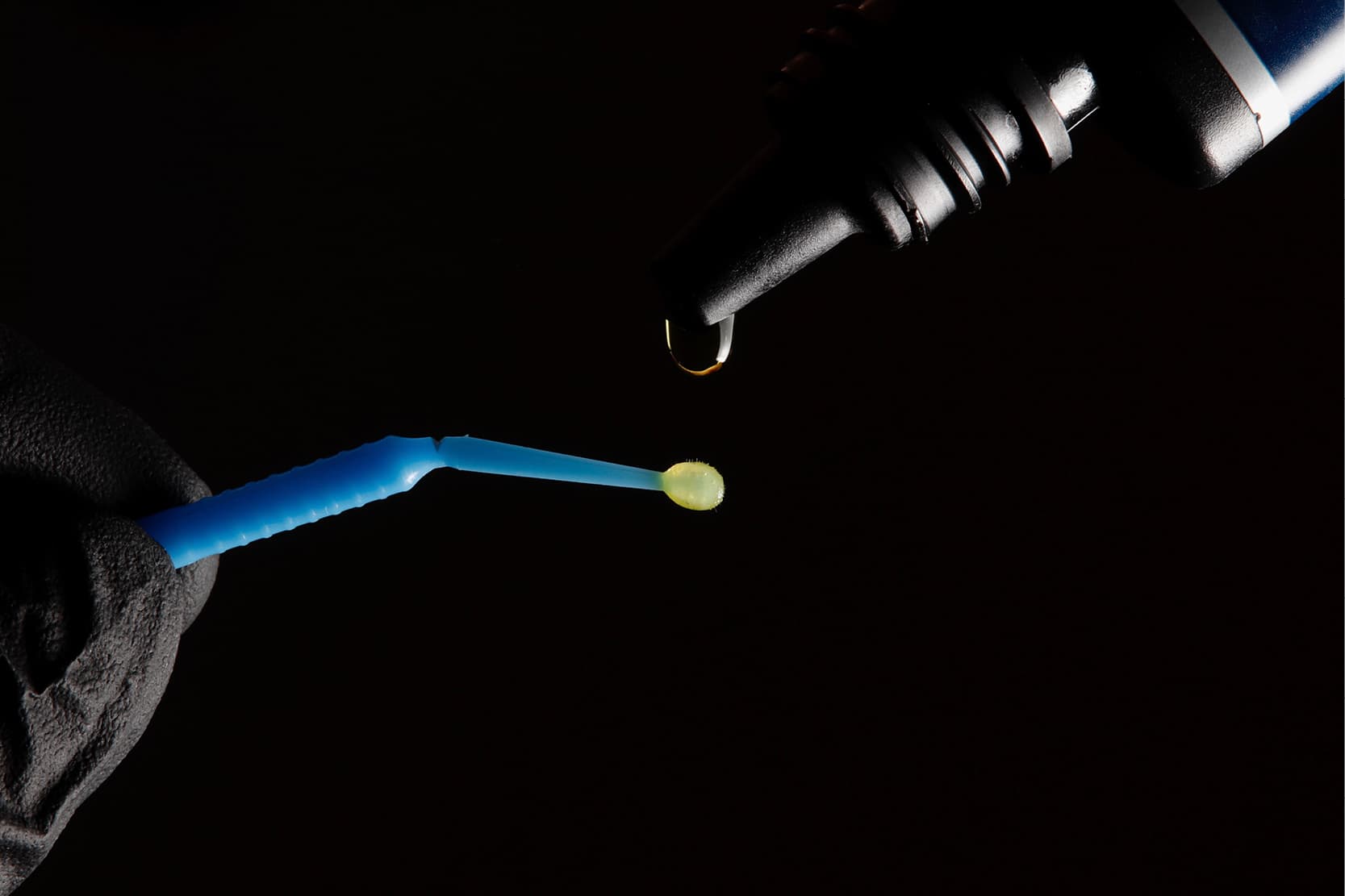
Adhesion to enamel is mainly based on micromechanical retention phenomena. The protocol involves etching with a strong acid (35–37% phosphoric acid), which selectively demineralises the enamel surface, dissolving the mineral content and creating a micro-rough surface with exposed prisms (3).
Adhesion to enamel is considered reliable and predictable due to the homogeneous nature of the tissue and the effectiveness of the acid etch. The shear bond strength values range from 20 to 30 MPa (4).
Mechanisms of adhesion to dentin
Adhesion to dentin is more complex than to enamel due to its heterogeneous structure, the greater proportion of organic components and its high water content. The main adhesion mechanism is based on the formation of the hybrid layer, a zone of demineralised collagen infiltrated by the resin, formed after acid conditioning (5).
The aim is to partially demineralise the intertubular dentin while preserving the architecture of the collagen matrix intact, allowing the resin monomers to infiltrate, forming a micromechanical interconnection.
Different factors can compromise the success of the dentin bond
- Presence of a Smear Layer: this forms during tooth preparation, obstructs the dentinal tubules and interferes with the penetration of the adhesive. Etch-and-rinse systems dissolve it by etching with a strong acid (6).
- Collagen collapse: excessive dehydration of the etched dentin during drying can cause the collagen matrix to collapse, hindering resin infiltration. It is essential to keep dentin properly moist in etch-and-rinse systems (7).
- Hydrophilicity/hydrophobicity of adhesives: adhesives must be sufficiently hydrophilic to infiltrate the moist dentin matrix. However, excessive hydrophilicity can lead to water absorption and reduced durability over time (8).
- Nanoleakage: incomplete infiltration or defective polymerisation can cause micro-gaps in the hybrid layer, compromising the long-term effectiveness of adhesion (9).
Bond durability
Degradation of the adhesive bond is a major concern. Enzymatic degradation of exposed collagen by matrix metalloproteinases (MMPs) and hydrolysis of the adhesive resin compromise the integrity of the bond.
The various strategies aimed at improving the durability of the adhesive bond include the use of MMP inhibitors (e.g., chlorhexidine), chemically more stable monomers (e.g., MDP) and the optimisation of the formation of the hybrid layer (10).
Studies show that while initial bond strength may be similar between different systems, its durability can vary significantly. Self-etch adhesives appear to offer better long-term performance due to less aggressive demineralisation and more homogeneous infiltration (11).
Clinical implications and future perspectives
Effective adhesion to enamel and dentin is critical to the success of direct and indirect restorations, such as composite fillings, inlays, veneers and crowns.
The choice of adhesive and the correct application technique are essential to prevent problems such as marginal discolouration, post-operative sensitivity and restoration failure.
Research in the field of dental adhesives is constantly evolving. Biomimetic approaches aim to replicate the natural structure of the dentin-enamel junction to improve performance. A deeper understanding of dentin biology and hybrid layer dynamics will likely lead to the development of more durable and less technique-sensitive adhesives.
- Ten Cate, A. R. (2013). Oral Histology: Development, Structure and Function (7th ed.). Elsevier.
- Pashley, D. H., et al. (2011). State of the art etch-and-rinse adhesives. Dental Materials, 27(1), 1–16.
- Buonocore, M. G. (1955). A simple method of increasing the adhesion of acrylic filling materials to enamel surfaces. Journal of Dental Research, 34(6), 849–853.
- Perdigão, J. (2010). Dentin bonding—Variables related to the clinical situation and the substrate treatment. Dental Materials, 26(2), e24–e37.
- Nakabayashi, N., et al. (1982). The promotion of adhesion by the infiltration of monomers into tooth substrates. Journal of Biomedical Materials Research, 16(3), 265–273.
- Pashley, D. H., et al. (2007). Collagen degradation by host-derived enzymes during aging. Journal of Dental Research, 86(8), 745–759.
- Tay, F. R., & Pashley, D. H. (2003). Have dentin adhesives become too hydrophilic? Journal of the Canadian Dental Association, 69(11), 726–731.
- Carrilho, M. R., et al. (2005). Durability of resin-dentin bonds related to water and oil storage. Journal of Dental Research, 84(11), 1040–1044.
- Hashimoto, M., et al. (2002). In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. Journal of Dental Research, 81(8), 556–560.
- Hebling, J., et al. (2005). Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. Journal of Dental Research, 84(8), 741–746.
Would you like more information about Zhermack Dental products and solutions?
Contact us



 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


