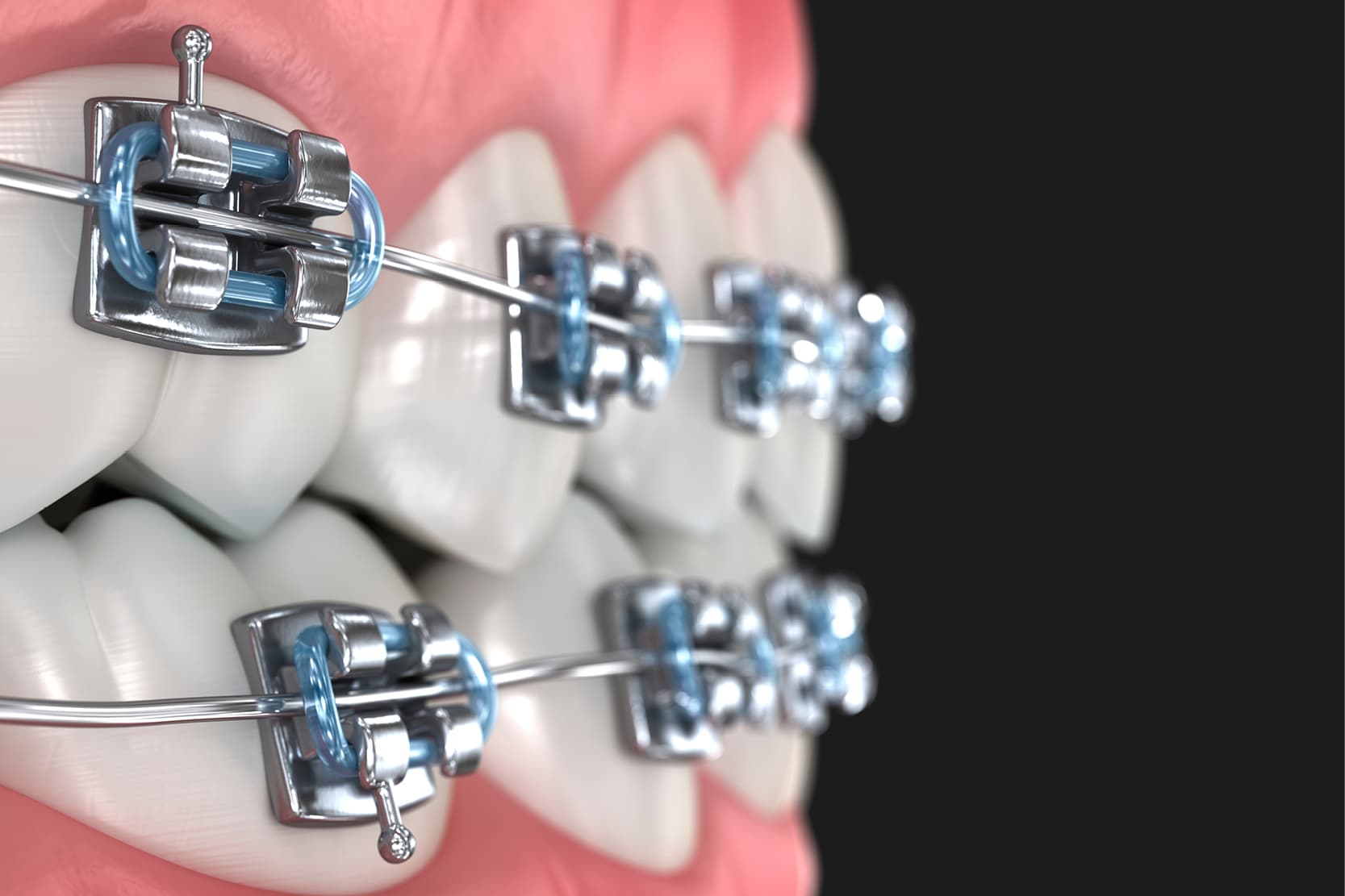
Dental rehabilitation procedures, especially those involving fixed or removable prosthetics, are highly dependent on the patient’s pre-existing dentition and occlusion. However, malocclusions, tooth inclinations, edentulous spaces and irregular occlusal planes often complicate prosthetic rehabilitation.
Pre-prosthetic orthodontics addresses these issues by correcting dental and skeletal abnormalities to establish a favourable environment for the prosthesis (1).
Pre-prosthetic orthodontics is essential to ensure that the prosthetic result is functional, aesthetically pleasing and biomechanically stable. By aligning the teeth, levelling the arches and optimising spaces, orthodontics facilitates the ideal positioning of prosthetic elements, the distribution of loads and oral hygiene access (2).
Malpositions such as tilted, rotated, over-erupted teeth or insufficient spaces can compromise the longevity of the prosthesis and increase the risk of mechanical or biological failure (3).
Clinical indications: when pre-prosthetic orthodontics is indicated
Redistribution of prosthetic spaces
In patients with missing teeth, adjacent teeth may tilt or migrate into the edentulous space, making any prosthetic rehabilitation more complex. Any dento-dental or dento-skeletal discrepancies requiring additive prosthetic rehabilitation solutions can benefit from a prosthetically guided orthodontic redistribution of the spaces. (4).
When we have excess space and therefore diastemata, through orthodontic therapy we can redistribute the interdental spaces to where they can be most useful for prosthetic purposes.
Crowding, misalignments, rotations and dental malpositions should always be corrected before the prosthetic phase itself, since the abutment preparations will be less invasive when avoiding the need for prosthetic modification of the position and angle of the teeth with the preparation drill. In this case, prosthetically guided orthodontics is particularly useful as it is less invasive and allows for better results during prosthetic rehabilitation. (5)
Uprighting the molars
The most classic example of preprosthetic orthodontics is represented by molar uprighting. It is very common, in fact, that following the extraction of a first or second molar, the element distal to the gap tends to become very markedly inclined mesially over the years.
When the interdental space is partially reduced and the angle of the element with respect to the occlusal plane becomes excessive, an exclusively prosthetic rehabilitation becomes very complex and can be expected to have a non-optimal result due to the need for some anatomical-functional compromise.
Tipped molars can hinder the placement of implants or bridges. Straightening improves axial alignment and also allows for better load distribution (6).
Dental intrusion
Another typical situation is the prolonged lack of opposing teeth. In this case, the elements of an arch tend to overerupt. As the teeth overerupt, they will no longer have physiological contact points, and interproximal spaces will form, within which plaque and tartar can accumulate, and periodontal pockets may form.
The overeruption of a tooth causes significant reduction in the available prosthetic space in the opposing arch; this process can be so significant as to make prosthetic rehabilitation of the gap impossible with a fixed prosthesis, whether on natural teeth or on implants. The orthodontic intrusion of over-erupted elements can re-establish the vertical spaces necessary to correctly rehabilitate the arch. (7).
Orthodontic extrusion
A crown-root fracture of an element, especially when the fracture line is subgingival, is a difficult event to manage clinically. One therapeutic option in these cases is the orthodontic extrusion. By extruding the element from its alveolus, in fact, it is possible to expose the fracture line at the supragingival level, thereby making its correct prosthetic rehabilitation possible.
This technique can also be useful for managing the verticality of bone and gingival volumes in view of implant-prosthetic rehabilitation (8) and for restoring a gingival parabola or an interproximal papilla compromised by periodontal problems.
Verticality management
Occlusal discrepancies such as deep or open bite can alter the prosthetic vertical dimension. Orthodontics allows the opening or closing of the bite to facilitate the integration of the prosthesis (9). It is also possible to partially address vertical problems such as some types of gummy smile by orthodontic treatment. (10)
Levelling of the occlusal plane
Irregular occlusal planes hinder the fit and functionality of the prosthesis. Pre-prosthetic orthodontics can level these planes (11).
In conclusion, to date, orthodontics and prosthetics are intimately linked. Knowing the potential of orthodontic treatment before embarking on rehabilitation therapy broadens the range of clinical solutions.
A prosthetically guided orthodontic approach is extremely effective and allows for better functional and aesthetic results, while minimising the invasiveness of treatments.
- Gillen, R. J., Schwartz, R. S., Hilton, T. J., & Evans, D. B. (2019). Interdisciplinary management for prosthodontic patients: The role of orthodontics. Journal of Prosthetic Dentistry, 121(5), 739–748. https://doi.org/10.1016/j.prosdent.2018.07.011
- Proffit, W. R., Fields, H. W., & Larson, B. (2018). Contemporary Orthodontics (6th ed.). Elsevier.
- Rinchuse, D. J., & Kandasamy, S. (2020). Evidence-based considerations for molar uprighting mechanics. Australian Orthodontic Journal, 36(1), 70–77.
- Papageorgiou, S. N., Gölz, L., Jäger, A., & Eliades, T. (2017). Clinical effectiveness of orthodontic treatment on patients’ quality of life: A systematic review and meta-analysis. Clinical Oral Investigations, 21(3), 543–554. https://doi.org/10.1007/s00784-016-1938-5
- Venezia P, Ronsivalle V, Isola G, Ruiz F, Casiello E, Leonardi R, Lo Giudice A. Prosthetically Guided Orthodontics (PGO): A Personalized Clinical Approach for Aesthetic Solutions Using Digital Technology. J Pers Med. 2022 Oct 14;12(10):1716. doi: 10.3390/jpm12101716. PMID: 36294855; PMCID: PMC9605514.
- Cheung, L. K., Wong, M. C., & Yiu, K. H. (2021). Orthodontic treatment prior to dental implants: A systematic review. Clinical Oral Implants Research, 32(4), 509–520. https://doi.org/10.1111/clr.13739
- Gross, M. D., Mardinger, O., & Nissan, J. (2020). The use of orthodontics in implant site development. Journal of Periodontology, 91(5), 587–595. https://doi.org/10.1002/JPER.19-0421
- González-Martín O, Solano-Hernandez B, Torres Muñoz A, González-Martín S, Avila-Ortiz G. Orthodontic Extrusion: Guidelines for Contemporary Clinical Practice. Int J Periodontics Restorative Dent. 2020 Sep/Oct;40(5):667-676. doi: 10.11607/prd.4789. PMID: 32925996.
- Nanda, R. (2021). Esthetics and Biomechanics in Orthodontics (2nd ed.). Elsevier Health Sciences.
- Inchingolo AD, Inchingolo AM, Viapiano F, Netti A, Ciocia AM, Ferrara I, Mancini A, Palermo A, Inchingolo F, Dipalma G. Effectiveness and Personalized Approaches in the Correction of Gummy Smile: A Systematic Review of Orthodontic and Surgical Treatments. J Clin Med. 2024 Nov 14;13(22):6843. doi: 10.3390/jcm13226843. PMID: 39597985; PMCID: PMC11594777.
- Kokich, V. O., & Spear, F. M. (2018). Guidelines for managing the orthodontic-restorative patient. Seminars in Orthodontics, 24(2), 125–134. https://doi.org/10.1053/j.sodo.2018.02.004
Would you like more information about Zhermack Dental products and solutions?
Contact us



 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


