
When producing prostheses for natural teeth, an impression has to be taken that accurately reproduces the one or more abutments concerned along with the adjacent teeth in the same arch.
To do so, the dentist needs to achieve a number of important prerequisites:
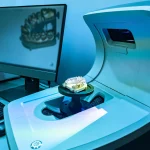
- the prosthetic margin of the preparation must be rendered adequately visible to the operator and accessible to the impression material or the light of the intraoral scanner if digital impression techniques are adopted;
- all humidity and films of saliva, blood or other fluids must be reduced to a minimum or ideally eliminated around the prepared teeth;
- soft tissues have to be displaced enough to give the impression material free access to the margin of the preparation.
To attain these results in daily clinical practice, dentists use tissue management techniques of three main types: mechanical, mechanical-chemical, and surgical.
Astringent, haemostatic and vasoconstrictor agents are all used in the mechanical-chemical technique. These agents assist the mechanical compression applied by the retraction cord to the single or double gingival sulcus prior to taking the impression with silicones, and promote the retraction of the soft tissues adjacent to the abutment.
However, the use of cotton retractor cord alone, without auxiliary chemical additives, has proved ineffective it often fails to stem subgingival bleeding [1]. In a study of the various methods of gingival retraction, Pelzner et al show that almost half of the impressions taken using retraction cord alone need to be repeated, as the procedure fails to reveal the limit of the preparation in the resulting stone model [2].
Mechanical-chemical tissue retraction is therefore the most commonly used technique today. In this technique, prior to insertion into the sulcus, the retractor cord is immersed in a solution containing astringent, haemostatic or vasoconstrictor agents. Such agents may be Class I (vasoconstrictor, adrenergic), or Class II (haemostatic, astringent) [3] depending on their oxidoreduction potential.
Common chemical compounds
Astringents like alum or aluminium and potassium sulphate (KAl (SO4)2), AlCl3 and zinc chloride (ZnCl2) are substances that precipitate proteins but do not penetrate the cells and therefore affect only the surface of the mucosa.
They harden this surface, making it mechanically more resistant and reducing mucosal exudation. Certain astringents, such as ferric chloride and ferric sulphate, are available in a more concentrated form (as haemostatic agents) and cause local surface coagulation of the blood [4].
Ferric sulphate, however, is no longer commonly used as it inhibits the polymerisation of the polyethers and is associated with tissue staining [5].
Aluminium chloride and ferrous sulphate are the most popular astringents as they cause less tissue damage and are both effective and easy to use [6]. Various haemostatic agents can stop the more serious haemorrhaging that occurs if capillaries or arterioles are cut.
Vasoconstrictors, on the other hand, do not cause blood coagulation but act by constricting the blood vessels themselves. Vasoconstrictors approved by the Council on Dental Therapeutics include: epinephrine (1:200,00/1:100,00/1:50,00), levonordefrin (1:20,00) and norepinephrine (1:30,00).
An 8% solution of racemic epinephrine is the go-to vasoconstrictor in dentistry [7,8]. It inhibits bleeding by reducing the diameter of the capillaries and thereby impeding subgingival haemorrhaging.
This local vasoconstrictor action also determines a temporary retraction of the gums that is useful during impression taking as it helps reveal the margin of the preparation [9]. Epinephrine must, however, be used for gingival retraction purposes only at a very low concentration (0.01%) because of the significant ischemic effect it produces in the soft tissues of the gingival sulcus.
Another inconvenience associated with epinephrine is its possible absorption and introduction into the systemic circulation. The amount of epinephrine absorbed can vary dramatically and depends on:
- the level of exposure of the vascular bed, which in turn depends on tissue inflammation [10];
- contact time [11];
- the degree of cord medication [12].
It is worth considering that 71 µg of epinephrine [13] is absorbed from 2.5 cm of retraction cord left in the gingival sulcus for 5 to 15 minutes and that this quantity corresponds to about 1/3 of the maximum recommended dose for a healthy adult (0.2 mg or 200 µg) and about twice the recommended dose for a cardiopathic patient (40 µg) [14].
When choosing astringent, haemostatic and vasoconstrictor agents, it is also important to verify their compatibility with the impression materials used. Some substances can interfere with the polymerisation of impression materials and significantly extend curing times.
This can lead to the impression material distorting or tearing right at the finish line (preparation margin) during removal from the patient’s mouth, as a result of insufficient curing and the necessary mechanical properties being only partly developed.
For this reason it is essential to choose an astringent/haemostatic/vasoconstrictor that is suitable both for the clinical case and for the impression material used. Choosing the wrong agent can easily compromise results and possibly even have a clinical impact.
It is important to remember that ferric sulphate and aluminium chloride interfere with the polymerisation of polyethers while aluminium sulphate can interfere with the polymerisation of addition silicones [5]. Epinephrine, on the other hand, does not interact negatively either with polyethers or polyvinylsiloxanes.
To eliminate any fluids that might inhibit curing, along with any coagulated blood deposits, it is highly recommended to rinse the gingival sulcus abundantly just prior to taking the impression [5].
It is also essential to use only the minimum quantity of these compounds necessary to obtain the desired haemostatic effect. Only in this way can the dental practitioner obtain a correct impression without causing tissue damage or compromising the impression material during anatomical registrations.

Tissue management prior to impression taking
Bibliography:
[1] Harrison JD. Effect of retraction materials on the gingival sulcus epithelium. The Journal of Prosthetic Dentistry 1961;11:514–21. https://doi.org/10.1016/0022-3913(61)90234-7.
[2] Pelzner RB, Kempler D, Stark MM, Lum LB, Nicholson RJ, Soelberg KB. Human blood pressure and pulse rate response to racemic epinephrine retraction cord. J Prosthet Dent 1978;39:287–92. https://doi.org/10.1016/s0022-3913(78)80098-5.
[3] Nowakowska D, Saczko J, Kulbacka J, Choromanska A. Dynamic oxidoreductive potential of astringent retraction agents. Folia Biol (Praha) 2010;56:263–8.
[4] Mohan M. Pharmacological Agents in Dentistry: A Review. BJPR 2011;1:66–87. https://doi.org/10.9734/BJPR/2011/272.
[5] Gherlone E. L’impronta in protesi dentaria. Masson, 2005. n.d.
[6] Rosenstiel, S.F., Land, M.F., Fujimoto, J. (2006a). Contemporary fixed prosthodontics 4thEdn. St Louis: Mosby, pp. 435. n.d.
[7] Felpel LP. A review of pharmacotherapeutics for prosthetic dentistry: Part I. J Prosthet Dent 1997;77:285–92. https://doi.org/10.1016/s0022-3913(97)70186-0.
[8] Shillinburg HT, et al. Fundamentals of fixed prosthodontics. Quintessence Publishing Company, 1997 n.d.
[9] Shillingburg HT, Hatch RA, Keenan MP, Hemphill MW. Impression materials and techniques used for cast restorations in eight states. J Am Dent Assoc 1980;100:696–9. https://doi.org/10.14219/jada.archive.1980.0228.
[10] Gogerty JH, Strand HA, Ogilvie AL, Dille JM. Vasopressor effects of topical epinephrine in certain dental procedures. Oral Surg Oral Med Oral Pathol 1957;10:614–22. https://doi.org/10.1016/s0030-4220(57)80009-7.
[11] Woycheshin FF. An evaluation of the drugs used for gingival retraction. The Journal of Prosthetic Dentistry 1964;14:769–76. https://doi.org/10.1016/0022-3913(64)90213-6.
[12] Forsyth RP, Stark MM, Nicholson RJ, Peng CT. Blood pressure responses to epinephrine-treated gingival retraction strings in the rhesus monkey. J Am Dent Assoc 1969;78:1315–9. https://doi.org/10.14219/jada.archive.1969.0186.
[13] Kellam SA, Smith JR, Scheffel SJ. Epinephrine absorption from commercial gingival retraction cords in clinical patients. J Prosthet Dent 1992;68:761–5. https://doi.org/10.1016/0022-3913(92)90198-j.
[14] Malamed SF. Medical Emergencies in the Dental Office, ed 6. St Louis: Mosby,2007:31;381-384. n.d.
Do you want more information on Zhermack Dental products and solutions?
Contact us



 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


