Impressions for edentulous patients are an extensively debated topic and the schools of thought among clinicians vary considerably [1].
In today’s scientific literature, several studies have compared digital and analogue impressions, focusing primarily on dentulous and implanted patients [2–5].
There are, however, far fewer studies comparing analogue and digital impressions in edentulous patients, particularly in-vivo [6]. Nevertheless, most of them agree on the inferiority of digital vs analogue impressions in these clinical cases [7–9].
Two-phase impressions are still the gold standard
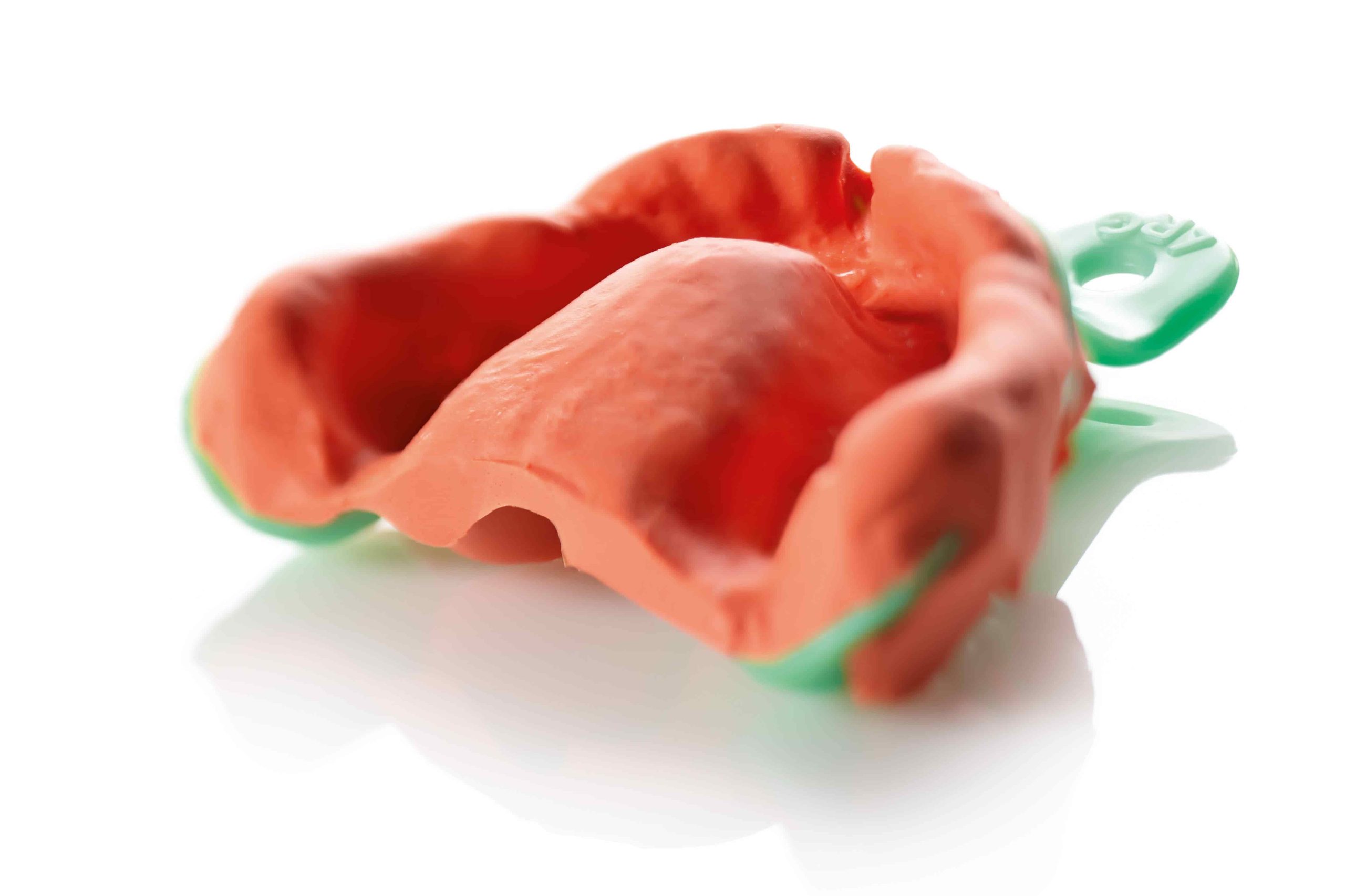
Current analogue protocols for impression-taking in edentulous patients involve recording the functional peripheral margins and the surface of the palatal mucosa with that of the alveolar crests either in two separate phases or in a single step [1].
Although there is still a certain amount of confusion regarding the need for a two-phase technique for edentulous patients, since some studies have shown that there are no patient-perceived differences following the fabrication of the removable restoration [10–12], the two-phase impression technique remains the gold standard.
The first phase consists in taking a functional impression of the peripheral seal area with thermoplastic paste, while the second step consists in taking an impression of the entire mucosal surface with zinc oxide eugenol (ZOE) or polysulphide paste [13].
The decision to use one or different materials and one or different techniques is therefore at the discretion of the dentist, who uses professional experience to choose the procedure that is most congenial to them, which is also often the most comfortable and affordable for the patient[14].
Digital impressions for edentulous patients: the critical aspects of intraoral scanning
Digital impressions, which are currently commonly used for dentulous and implant patients, are not yet universally recommended for edentulous patients [7–9].
Let’s take a closer look at the critical aspects regarding intraoral scanning.
Operational difficulties with mobile, mucosal and translucent tissues
Although it is able to scan soft tissues without any physical contact, making it possible to obtain an effective mucostatic impression[8], intraoral scanning is not suitable for obtaining proper functional impressions of the peripheral seal area [7–9].
Given their mechanism of acquiring and reconstructing images from reflected light, intraoral scanners are capable of scanning “static” structures, such as teeth or Scan Bodies on implants, but they encounter great difficulties with mobile or mucosal and translucent tissues [6,15,16].
Discrepancies between the measured and actual vestibular dimension
Taking impressions on the edentulous mucosa of an upper or lower arch also involves stretching the labial areas in order to introduce the intraoral scanner handpiece. This technical drawback, which is inevitable with intraoral scanning, results in a discrepancy between the measured and the actual vestibular dimension [7,8].
Therefore, the concept according to which the edge of the restoration must be in perfect harmony with muscle function [17] cannot be respected, making it impossible to create a true peripheral seal for the removable denture.
Adaptation to the free mucosa
Intraoral scanning of edentulous patients therefore makes it possible to achieve an extremely accurate and precise restoration at adherent mucosa level, but that does not adapt properly at free mucosa level [8,16,18,19].
Fabricating a removable denture at keratinised tissue level alone, is not, however, always possible, particularly when it is necessary to extend the margins and the flanges in order to ensure labial and aesthetic support or if the smile line is accentuated [20–22].
Stitching process errors
Furthermore, being a smooth, translucent and completely saliva-coated surface, the intraoral mucosa can generate errors in the stitching process the scanner performs to obtain the 3D scan [9].
Although these factors are important for the upper arch, they have an even greater impact when it comes to the mandible, where the lack of keratinised tissue, the palatal ridges and the presence of the tongue and saliva all contribute to significantly impairing scanner performance [18,23].
Want to find out more?
Discover the differences between preliminary and functional impressions for edentulous patients.
Present and future prospects for removable dentures in edentulous patients
With this in mind, it still seems difficult to fabricate removable dentures directly from intraoral scans on edentulous patients.
Future scanning technology capable of recording the thickness of the soft tissues in order to deduce their compressibility and the degree of tissue mobility could bridge the gap that currently separates digital impressions from analogue ones.
Zhermack provides a vast range of alginates with characteristics that are suited to use in edentulous patients for the fabrication of full removable dentures.
More specifically, Neocolloid is an alginate with a long setting time conceived to afford appropriate functional impressions following specific manoeuvres that mobilise the perioral soft tissues of edentulous patients.
Thanks to its physical and chemical characteristics, Neocolloid also allows excellent reproduction of the maxillary mucosae.
References
[1] Jayaraman S, Singh BP, Ramanathan B, Pazhaniappan Pillai M, MacDonald L, Kirubakaran R. Final-impression techniques and materials for making complete and removable partial dentures. Cochrane Database Syst Rev 2018;4:CD012256. https://doi.org/10.1002/14651858.CD012256.pub2.
[2] Alsharbaty MHM, Alikhasi M, Zarrati S, Shamshiri AR. A Clinical Comparative Study of 3‐Dimensional Accuracy between Digital and Conventional Implant Impression Techniques. Journal of Prosthodontics 2019;28:e902–8. https://doi.org/10.1111/jopr.12764.
[3] Bandiaky ON, Le Bars P, Gaudin A, Hardouin JB, Cheraud-Carpentier M, Mbodj EB, et al. Comparative assessment of complete-coverage, fixed tooth-supported prostheses fabricated from digital scans or conventional impressions: A systematic review and meta-analysis. J Prosthet Dent 2020:S0022-3913(20)30498-4. https://doi.org/10.1016/j.prosdent.2020.09.017.
[4] Celeghin G, Franceschetti G, Mobilio N, Fasiol A, Catapano S, Corsalini M, et al. Complete-Arch Accuracy of Four Intraoral Scanners: An In Vitro Study. Healthcare 2021;9:246. https://doi.org/10.3390/healthcare9030246.
[5] Grande F, Celeghin G, Gallinaro F, Mobilio N, Catapano S. Comparison of the accuracy between full-arch digital scans and scannable impression materials: an in vitro study. Minerva Dent Oral Sc 2023. https://doi.org/10.23736/S2724-6329.23.04766-6.
[6] Mangano F, Gandolfi A, Luongo G, Logozzo S. Intraoral scanners in dentistry: a review of the current literature. BMC Oral Health 2017;17:149. https://doi.org/10.1186/s12903-017-0442-x.
[7] D’Arienzo LF, D’Arienzo A, Borracchini A. Comparison of the suitability of intra-oral scanning with conventional impression of edentulous maxilla in vivo. A preliminary study. Journal of Osseointegration 2018;10:115–20. https://doi.org/10.23805/jo.2018.10.04.02.
[8] Chebib N, Kalberer N, Srinivasan M, Maniewicz S, Perneger T, Müller F. Edentulous jaw impression techniques: An in vivo comparison of trueness. J Prosthet Dent 2019;121:623–30. https://doi.org/10.1016/j.prosdent.2018.08.016.
[9] Rasaie V, Abduo J, Hashemi S. Accuracy of Intraoral Scanners for Recording the Denture Bearing Areas: A Systematic Review. Journal of Prosthodontics 2021:jopr.13345. https://doi.org/10.1111/jopr.13345.
[10] Komagamine Y, Kanazawa M, Sato Y, Iwaki M, Jo A, Minakuchi S. Masticatory performance of different impression methods for complete denture fabrication: A randomized controlled trial. J Dent 2019;83:7–11. https://doi.org/10.1016/j.jdent.2019.01.009.
[11] Albuquerque IS, Regis RR, de Souza RF, Gurgel KF, Silva PG, Pinto-Fiamengui LMS, et al. Is a two-step impression mandatory for complete denture fabrication on the severely resorbed mandible? A randomized trial on patient perception and denture quality. Journal of Dentistry 2020;98:103356. https://doi.org/10.1016/j.jdent.2020.103356.
[12] Hyde TP, McCord JF. Survey of prosthodontic impression procedures for complete dentures in general dental practice in the United Kingdom. The Journal of Prosthetic Dentistry 1999;81:295–9. https://doi.org/10.1016/S0022-3913(99)70272-6.
[13] Mehra M, Vahidi F, Berg RW. A Complete Denture Impression Technique Survey of Postdoctoral Prosthodontic Programs in the United States: Complete Denture Impression Technique Survey. Journal of Prosthodontics 2014;23:320–7. https://doi.org/10.1111/jopr.12099.
[14] Tsirogiannis P, Neophytou S, Reul A, Heydecke G, Reissmann DR. Can we measure patients’ perception during dental impressions? The Burdens in Dental Impression-Making Questionnaire – BiDIM-Q. Journal of Prosthodontic Research 2017;61:34–42. https://doi.org/10.1016/j.jpor.2016.03.003.
[15] Li H, Lyu P, Wang Y, Sun Y. Influence of object translucency on the scanning accuracy of a powder-free intraoral scanner: A laboratory study. J Prosthet Dent 2017;117:93–101. https://doi.org/10.1016/j.prosdent.2016.04.008.
[16] Maniewicz S, Imamura Y, El Osta N, Srinivasan M, Müller F, Chebib N. Fit and retention of complete denture bases: Part I – Conventional versus CAD-CAM methods: A clinical controlled crossover study. The Journal of Prosthetic Dentistry 2022. https://doi.org/10.1016/j.prosdent.2022.07.006.
[17] Moderno Trattato di protesi Mobile Completa [Glauco – Martina Edizioni] n.d. https://www.medicalinformation.it/moderno-trattato-di-protesi-mobile-completa-glauco-martina-edizioni-9788875721183glauco-marino-canton-alessandro-marino-antonino-di-lullo-nicola.html (accessed January 3, 2023).
[18] Lo Russo L, Caradonna G, Troiano G, Salamini A, Guida L, Ciavarella D. Three-dimensional differences between intraoral scans and conventional impressions of edentulous jaws: A clinical study. J Prosthet Dent 2020;123:264–8. https://doi.org/10.1016/j.prosdent.2019.04.004.
[19] Grande F, Tesini F, Pozzan MC, Zamperoli EM, Carossa M, Catapano S. Comparison of the Accuracy between Denture Bases Produced by Subtractive and Additive Manufacturing Methods: A Pilot Study. Prosthesis 2022;4:151–9. https://doi.org/10.3390/prosthesis4020015.
[20] Lombardi RE. The principles of visual perception and their clinical application to denture esthetics. The Journal of Prosthetic Dentistry 1973;29:358–82. https://doi.org/10.1016/S0022-3913(73)80013-7.
[21] Avrampou M, Mericske-Stern R, Blatz MB, Katsoulis J. Virtual implant planning in the edentulous maxilla: criteria for decision making of prosthesis design. Clin Oral Implants Res 2013;24 Suppl A100:152–9. https://doi.org/10.1111/j.1600-0501.2011.02407.x.
[22] Montanari M, Tallarico M, Vaccaro G, Ferrari E, Scrascia R, Ortensi L, et al. Two Years after Loading Performance of Implant-Supported Overdenture with Metal Bar and Low-Profile Attachments: A Prospective Case Series Multicenter Clinical Study. International Journal of Dentistry 2020;2020:1–8. https://doi.org/10.1155/2020/8830722.
[23] Hack G, Liberman L, Vach K, Tchorz JP, Kohal RJ, Patzelt SBM. Computerized optical impression making of edentulous jaws – An in vivo feasibility study. J Prosthodont Res 2020;64:444–53. https://doi.org/10.1016/j.jpor.2019.12.003.
Do you want more information on Zhermack Dental products and solutions?
Contact us




 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


