
Tooth loss, whether due to trauma, developmental abnormalities or pathological conditions, is an extremely common problem that affects individuals of all ages.
Traditional methods of tooth replacement such as prosthetics on natural teeth or implant prosthetics offer functional solutions, but each has inherent limitations.
In this context, the autotransplantation of teeth has evolved as a promising alternative, with the potential to preserve both architecture and functionality.
The technique involves the transfer of a donor tooth, often a third molar or premolar, to replace a missing or damaged tooth.
Dental autotransplantation technique
The dental autotransplantation process typically involves several stages, including:
- Extraction of the tooth;
- Preparation of the site;
- Transplantation of the tooth;
- Post-operative care (1).
The donor tooth, often a third molar or premolar, is extracted while attempting to preserve the periodontal ligament, which plays a crucial role in revascularisation and integration into the recipient site (2).
Once extracted, the tooth is carefully inserted into the prepared recipient site, which is usually the post-extraction socket of a lost tooth. The next step involves splinting the tooth to neighbouring teeth to stabilise it during the healing process.
Two key aspects: timing and preparation
One essential aspect of the procedure is the timing of the transplant. Successful outcomes are more likely when the donor tooth is transplanted immediately after extraction, as prolonged extraoral time may lead to complications such as root resorption (3).
Some studies suggest that transplantation should occur within 15-20 minutes of extraction to minimise damage to the periodontal ligament (4).
In addition to the timing of the procedure, site preparation is critical to success. The recipient site must be carefully prepared to ensure that the donor tooth fits properly and that the root surfaces are free of contamination (5).
Several techniques, including the use of saline or specialised growth factors, may be used to promote healing and reduce the risk of complications.
Tooth autotransplantation: factors that influence success
The success of tooth autotransplantation is influenced by a number of factors, ranging from specific patient characteristics to surgical variables.
A review of the literature has highlighted several success factors, including the age of the patient, the type of tooth transplanted, the quality of the periodontal ligament and the surgical technique used.
1) Patient’s age
Age is one of the most significant factors influencing the success of tooth autotransplantation.
Younger patients, particularly those between the ages of 10 and 25, tend to have higher success rates due to the greater root development capacity and robust healing capacity of their periodontal tissues (6).
Conversely, older patients may have lower success rates due to reduced periodontal ligament vitality and slower healing processes (7).
2) Type of tooth
The type of tooth transplanted also plays a role in the procedure’s success.
Third molars (wisdom teeth) are the most commonly used donor teeth, as they are often extracted for orthodontic reasons and are suitable for transplantation.
However, some studies indicate that the success rate may vary depending on the type of tooth.
For example, premolars have a higher success rate than molars due to their smaller root surface and better adaptability to the recipient site (3).
3) Condition of the periodontal ligament (PDL)
The condition of the periodontal ligament is another crucial factor.
The periodontal ligament plays a fundamental role in the revascularization and reattachment of the tooth to the alveolar bone. Damage to the PDL during tooth extraction or prolonged extraoral time may compromise the success of the transplant (2).
Studies suggest that teeth with an intact, healthy PDL have higher survival rates after transplantation than those with a damaged or necrotic PDL (5).
4) Surgical technique and post-operative care
Correct surgical technique is essential for the success of tooth autotransplantation.
Ensuring minimal trauma to the periodontal ligament, the correct position of the donor tooth and effective splinting are essential steps in achieving positive outcomes (1).
Post-operative care, which includes the use of antibiotics, pain management and regular follow-up visits, is equally crucial in preventing complications such as infections, root resorption or tooth loss (4).
Complications of tooth autotransplantation
While tooth autotransplantation has a high success rate in many cases, it can cause some complications.
The most common problems include:
- root resorption;
- infections;
- ankylosis.
Root resorption is a significant concern after transplantation and can lead to tooth loss (7). The early identification of root resorption and appropriate management, such as radiographic imaging monitoring, are crucial in preventing long-term complications.
Ankylosis is another potential complication, especially when there is excessive damage to the periodontal ligament or if the tooth is not positioned correctly in the recipient site.
Future possibilities
Recent advances in regenerative medicine and tissue engineeringoffer promising opportunities to improve the outcomes of tooth transplantation.
Techniques such as the use of stem cells and biomaterial scaffolds forperiodontal ligament regeneration could improve healing and revascularisation of transplanted teeth (3).
Furthermore, the development of advanced imaging techniques for pre-operative planning and post-operative monitoring could enable more precise surgical interventions, leading to better long-term outcomes.
In conclusion, tooth autotransplantation appears to be a promising and interesting technique, especially in young patients with healthy donor teeth.
The success of the procedure depends on several factors, including the patient’s age, the type of tooth, the health of the periodontal ligament (PDL) and the surgical technique. Despite potential complications such as root resorption and ankylosis, with proper management autotransplantation can be a viable alternative to conventional prosthetic options.
Further research into regenerative approaches and surgical advancements will likely continue to improve the success rates and clinical outcomes of this procedure.
References
- Li, X., Zhang, H., & Yang, Z. (2021). Surgical techniques and outcomes of teeth autotransplantation: A 5-year follow-up study. International Journal of Oral and Maxillofacial Surgery, 50(9), 1124-1130. https://doi.org/10.1016/j.ijom.2021.04.005
- Lindh, C., & Petersson, A. (2018). The role of the periodontal ligament in the success of tooth transplantation. Journal of Periodontology, 89(1), 112-119.
- Wu, Y., Chen, J., Xie, F., Liu, H., Niu, G., & Zhou, L. (2019). Autotransplantation of mature impacted tooth to a fresh molar socket using a 3D replica and guided bone regeneration: two years retrospective case series. BMC Oral Health, 19, 1-8.
- Galler, K. M., & Dohle, E. (2020). Postoperative care and complications following teeth autotransplantation: A clinical guide. Clinical Oral Investigations, 24(2), 447-457. https://doi.org/10.1007/s00784-019-03127-6
- Alhaddad, S., Moghaddam, M. A., & Shahnazari, M. (2020). Success factors in teeth autotransplantation: A systematic review. Journal of Oral and Maxillofacial Surgery, 78(8), 1523-1534. https://doi.org/10.1016/j.joms.2020.04.033
- Kokich, V. G. (2015). Autotransplantation of teeth: Indications, technique, and prognosis. Journal of Clinical Orthodontics, 49(5), 302-309. https://doi.org/10.2319/0514-348
- Bjerklin, K., & Nilsson, J. (2016). Autotransplantation of teeth: A retrospective study of 200 cases. European Journal of Orthodontics, 38(3), 288-295. https://doi.org/10.1093/ejo/cjw057
Would you like more information about Zhermack Dental products and solutions?
Contact us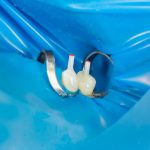




 Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.
Zhermack SpA has been one of the most important producers and international distributors of alginates, gypsums and silicone compounds for the dental sector for over 40 years. It has also developed solutions for the industrial and wellbeing sectors.
Zhermack SpA - Via Bovazecchino, 100 - 45021 Badia Polesine (RO), Italy.


